Abstract
Background
This study aims to: (1) examine rates of obesity and physical health complaints among 911 telecommunicators; and (2) document the role of emotion dysregulation, psychological inflexibility, duty-related distress and dissociation, and psychopathology in predicting obesity and physical health complaints in this population.
Methods
The sample consisted of 911 telecommunicators from across the country (N = 758). Participants completed an online survey assessing their mental and physical health functioning.
Results
A total of 82.5% of the sample reported a body mass index that fell within the overweight or obese category and an average of 17 physical health complaints within the past month. Peritraumatic reactions (distress and dissociation), emotion dysregulation, and psychological inflexibility had effects on physical health largely through psychopathology (alcohol abuse, post-traumatic stress disorder, and depression).
Conclusion
Development of adapted prevention and intervention efforts with this population is needed.
Keywords: obesity, peritraumatic distress, psychopathology, 911 telecommunicators
1. Introduction
Emergency responders provide critical services that are relied upon for the health and safety of the public. These occupations are characterized by routine exposure to psychological stressors, high levels of work demand, and risk for poor mental and physical health [1], [2]. The majority of literature on first responders has focused on police officers, firefighters, and emergency medical technicians. Less is known in regard to the health consequences of work for 911 telecommunicators, a group that sets the emergency responding chain in motion. Telecommunicators are relied upon by the public to assess the nature of the emergency, the type of response needed, and they dispatch appropriate help, all within minutes of answering a call. Although research has recently begun to explore the health impact of this occupation, substantial gaps in the literature exist.
Exposure to occupational stressors has been associated with a range of mental health consequences for first responders. Alcohol abuse, for example, is prevalent among firefighters [3], [4], police officers [5], [6], and first responders who were involved in recovery efforts following Hurricane Katrina [7]. Research has also shown enhanced risk for depressive symptoms in firefighters [4], [8], police officers [9], and emergency workers responding to Hurricane Katrina [7] and the terrorist attacks of 9/11 [10]. Additionally, there is considerable research documenting an increased risk for posttraumatic stress disorder (PTSD) among first responders [8], [11], [12]. Although limited, research has also provided evidence that the stressors faced by telecommunicators may lead to the development of depressive symptoms and PTSD in this population [13].
Poor physical health has also been documented among first responders. These occupations are typically associated with nonstandard schedules (i.e., shifts other than 9.00 am to 5.00 pm) and mandatory overtime [14], [15]. Shift work has been recognized as a risk factor for sleep disruption, metabolic syndrome, cardiovascular disease, and diabetes [9], [16]. Recent research has begun to investigate these associations among first responders, particularly with metabolic syndrome and weight issues. One recent study investigated the prevalence of metabolic syndrome among police officers with varying work schedules. Violanti et al [17] found that 62.2% of the police officers reported at least one component of metabolic syndrome, with reduced high density lipoprotein cholesterol (38.8%), elevated waist circumference (30.6%), and glucose intolerance (21.4%) being the most prevalent individual components. Research on metabolic syndrome among firefighters has found similar rates, with 73% of firefighters in one study reporting at least one component of metabolic syndrome [18].
Given these findings, it is unsurprising that a high percentage of emergency responders are overweight and/or obese. One recent study found that the prevalence rate of being overweight or obese [using a body mass index (BMI) ≥ 30 kg/m2] among career (79.5%) and volunteer (78.4%) firefighters was higher than the United States general adult population [19]. Additionally, research has shown high rates of excess weight and elevated cardiovascular risk among emergency responder candidates, including ambulance personnel [2]. To date, no research has examined the prevalence of obesity and physical health complaints among 911 telecommunicators. This gap is particularly important to address given that police officers, firefighters, and ambulance personnel are often more physically active at work than telecommunicators, which may buffer against poor physical health and weight problems.
Notably, pathology such as alcohol abuse, depression, and PTSD have been shown to contribute to many of the negative physical health consequences (i.e., weight problems and physical health complaints) common among first responders. Problematic use or excessive intake of alcohol is associated with increased caloric intake, which has been linked to higher BMI and risk for obesity [20]. There are mixed findings in regard to the relationship between obesity and depression; however, the majority of the research has pointed to a direct relationship between depressive symptoms and obesity [21]. In a large nationally representative survey with police officers, results showed that psychological distress, defined as the presence of depressive symptoms, anxiety symptoms, and/or fatigue, was associated with increased BMI among women officers in general, and among men officers reporting low physical activity [22]. Additionally, in a sample of firefighters, depression was associated with increased alcohol abuse as well as with increased sleep disruptions [4]. Moreover, research has shown that individuals suffering from PTSD have increased resting heart rate, heart rate reactivity, and increased startle response [23]. In a sample of police officers, Violanti et al [24] revealed that police officers with severe symptom levels of PTSD were approximately three times more likely to have metabolic syndrome (prevalence ration = 3.31) in comparison to police officers with low symptom levels. Given the relationship between mental and physical health, it is likely that etiological pathways are shared for first responders.
As research expands on the health outcomes of these occupations, it is important to identify vulnerability factors for first responders. Currently, research has focused primarily on predictors of psychopathology among first responders. Peritraumatic reactions, defined as the reactions during or in the immediate aftermath of trauma exposure, have been especially implicated in risk for post-trauma psychopathology. In fact, peritraumatic dissociation has been identified as the strongest predictor of post-trauma psychopathology (weighted r = 0.35) in a meta-analysis by Ozer et al [25]. Peritraumatic distress also showed a consistent relationship with PTSD symptomatology, with a weighted r = 0.26 [25]. Greater peritraumatic emotional distress and dissociation have been shown to predict depression and PTSD among firefighters, police officers, paramedics, and emergency medical technicians, as well as 911 telecommunicators [11], [26], [28], [27]. In regard to physical health, both peritraumatic dissociation and distress were found to be associated with somatization symptoms (i.e., physical health complaints) among women police officers [29]. The role of these reactions in physical health outcomes has not yet been explored among 911 telecommunicators.
Recent research has also illustrated the role of two other mechanisms, emotion dysregulation and psychological inflexibility, in psychological and physical health outcomes among individuals exposed to chronic occupational stress and trauma. Emotion dysregulation refers to difficulties in the multidimensional process that involves understanding, accepting, and modulating one's emotions to engage in appropriate goal-directed behaviors in response to environmental demands [30]. Given the emotionally intense and unpredictable nature of emergencies, the significance of one's ability to regulate emotions while at work is salient for first responders. Moreover, emotion regulation skills are implicated in buffering the impact of negative life-events and coping with occupational and environmental stressors. Previous studies have found that emotion dysregulation is associated with greater PTSD symptom severity [31], [32], [33], anxiety disorders, depression [34], and eating pathology [35].
Psychological flexibility is defined as how an individual adapts to fluctuating situational demands, reconfigures mental resources, shifts perspective, and maintains balance across life domains [36]. Kashdan and Rottenberg [36] refer to psychological flexibility as a key ingredient to overall health. Previous research has shown that inflexibility is associated with a variety of poor health outcomes [37], [38]. Difficulties with emotion regulation, as well as overall psychological inflexibility, may contribute to the poor psychological and physical health consequences of work among emergency responders. However, there has been limited research examining these factors among first responders. In a sample of police officers, Berking et al [39] found that, in comparison to civilians, the officers had difficulties accepting and tolerating negative emotions, engaging in compassionate self-support during distressing situations, and confronting situations that cue negative emotions. To date, no research has explored emotion regulation difficulties or psychological flexibility among telecommunicators.
The current study aimed to address several gaps in the literature surrounding the psychological and physical health of 911 telecommunicators. In a large sample of telecommunicators from across the country, physical health (BMI and physical health complaints) and psychological health (PTSD, depression, alcohol abuse) were assessed. In addition, telecommunicators' peritraumatic reactions (distress and dissociation) in relation to their worst duty-related call were measured, as well as their trait level of emotion dysregulation and psychological inflexibility. Using structural equation modeling, two models were posited with the following effects anticipated on the basis of prior research: (1) a significant direct effect of psychological inflexibility and emotion dysregulation on peritraumatic reactions, mental health, and physical health (e.g., BMI and physical health complaints); (2) a significant direct effect of peritraumatic reactions on mental health and physical health (e.g., BMI and physical health complaints); (3) a significant direct effect of mental health on physical health (e.g., BMI and physical health complaints); (4) a significant indirect effect of psychological inflexibility and emotion dysregulation on mental health via peritraumatic reactions; and (5) a significant indirect effect of psychological inflexibility and emotion dysregulation on physical health (e.g., BMI and physical health complaints) through mental health and peritraumatic reactions.
2. Materials and methods
2.1. Participants
Participants were 758 individuals with at least 1 year of experience as a telecommunicator. Ages ranged from 19 to 65 years [mean = 39.75 years, standard deviation (SD) = 9.73]. Consistent with previous samples of telecommunicators [13], the majority of the sample were women (73.7%) and most individuals identified as European American (88%). The majority of the sample had some college or vocational training (51.1%) or a college degree (31.4%). Most participants were married (53.2%) or living with a partner (12.3%). The average years of experience as a telecommunicator was 12.45 years (SD = 8.17).
2.2. Measures
2.2.1. Physical health
Body mass was calculated using the body mass index {i.e., [weight (lb)/height (in)2]*703}. Weight status was determined in accordance with the Centers for Disease Control and Prevention guidelines (www.cdc.gov/obesity). The Pennebacker Inventory of Limbic Languidness [40] is a 54-item measure that assesses the frequency of common physical complaints and sensations. A total score (α = 0.93) was calculated by summing the number of items the individual endorsed as having happened at least once in the past month.
2.2.2. Mental health
The Alcohol Use Disorders Identification Test [41] is a 10-item measure that was used to examine the extent of alcohol use problems. The Alcohol Use Disorders Identification Test has been used previously with police officers [42]. Scoring (α = 0.79) was completed in accordance with the procedures outlined by Babor et al [41], with higher scores indicating greater alcohol use problems. The Beck Depression Inventory-II (BDI-II) [43] is a widely used measure of depression and was used to assess the severity of depressive symptoms over the past 2 weeks. The BDI has been used in a variety of populations, including police officers [44] and has demonstrated adequate psychometric properties [45]. The BDI-II consists of 21 items that are summed to calculate a total symptom score (α = 0.93), with higher scores indicating greater depression. PTSD symptoms were measured with the PTSD Checklist—Civilian (PCL-C) [9]. The PCL-C is a 17-item measure that examines PTSD symptom severity in the past month; instructions were modified to specify experiences that occurred at work as a 911 telecommunicator. The PCL-C has been used in a variety of populations and has shown adequate psychometric properties [46]. A total symptom severity score (α = 0.94) was calculated by summing all items, with higher scores indicating greater PTSD symptomatology.
2.2.3. Duty-related experiences
The Peritraumatic Distress Inventory [47] is a 13-item measure used to assess distress associated with an identified “worst” duty-related incident. The Peritraumatic Distress Inventory has been used in previous research with 911 telecommunicators [26]. A total score (α = 0.81) was obtained by summing all items; higher scores indicated greater distress. The Peritraumatic Dissociative Experiences Questionnaire [48] is a 10-item measure that examines dissociative symptoms during an identified worst duty-related incident. The Peritraumatic Dissociative Experiences Questionnaire has been used previously with police officers [49]. A total score (α = 0.87) was calculated by summing all items, with higher scores indicating greater peritraumatic dissociation.
2.2.4. Emotion dysregulation
Emotion dysregulation was measured with the Difficulties in Emotion Regulation Scale (DERS) [30]. The DERS is a 36-item measure that is scored by reverse coding 11 negatively keyed items and summing responses. Five subscale scores [i.e., nonacceptance of emotional responses (α = 0.93), difficulties engaging in goal-directed behavior (α = 0.85), impulse control difficulties (α = 0.86), limited access to emotion regulation strategies (α = 0.89), and lack of emotional clarity (α = 0.84)] were obtained to examine different aspects of emotion dysregulation. Adequate psychometric properties of the DERS have been demonstrated in a variety of populations [50].
2.2.5. Psychological inflexibility
The Acceptance and Action Questionnaire-II [51] is a 7-item measure that was used to assess psychological inflexibility. The Acceptance and Action Questionnaire-II has previously demonstrated adequate psychometric properties [51]. A total score (α = 0.93) was calculated by summing all items, with higher scores indicating greater psychological inflexibility.
2.3. Procedure
Participants were recruited via advertisements sent to 911 telecommunication centers across the country, electronic mailing lists, and social media pages. Data collection occurred between June, 2013 and May, 2014. Participants were screened in an online survey to ensure all participants were older than 18 years and had at least 1 year of experience as a telecommunicator. Qualified participants were emailed the questionnaire's web address and unique login information. The informed consent and all questionnaires were completed online. Although completion time varied substantially, it took participants an average of 108 minutes to complete all questionnaires. Upon completion, participants were debriefed. At the end of data collection, 10 $100 cash prizes were drawn and distributed to winning participants. The study was approved by the Institutional Review Board at Northern Illinois University, DeKalb, USA.
3. Results
As anticipated, the rates of obesity were elevated in this population of emergency responders. In fact, use of a BMI cut-off score of 30 yielded an obesity prevalence rate of 53.4% (n = 405) in the sample. An additional 29.0% (n = 220) fell into the overweight category using a BMI range of 25–30 kg/m2, leaving only 17.5% (n = 133) in the normal to underweight categories. Though the general population of adults in the United States suffers from a high rate of obesity (34.9%) according to the Centers for Disease Control and Prevention (www.cdc.gov/obesity), the rate was nearly 50% greater among telecommunicators. When asked whether the participant had gained weight in the past 3 months, 52.2% (n = 396) reported that their weight had increased in the past 90 days, suggesting a sustained problem in this population. Further, participants had a mean score of 16.90 (SD = 10.76) on the PILL, suggesting an average of nearly 17 different physical health complaints that participants experienced at least “every month or so” up to “more than once every week.” Zero order correlations revealed an anticipated pattern of associations among key study variables based on previous research (Table 1).
Table 1.
Zero order correlations among key study variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BMI | — | ||||||||||||
| 2. Health complaints | 0.16* | — | |||||||||||
| 3. Alcohol use problems | −0.06 | 0.04 | — | ||||||||||
| 4. Depressive symptoms | 0.13* | 0.51* | 0.20* | — | |||||||||
| 5. PTSD symptoms | 0.08† | 0.47* | 0.15* | 0.64* | — | ||||||||
| 6. Peritraumatic dissociation | 0.05 | 0.33* | 0.07 | 0.36* | 0.49* | — | |||||||
| 7. Peritraumatic distress | 0.06 | 0.38* | 0.07 | 0.40* | 0.51* | 0.66* | — | ||||||
| 8. Psychological inflexibility | 0.07‡ | 0.44* | 0.18* | 0.74* | 0.58* | 0.37* | 0.41* | — | |||||
| 9. Nonacceptance | 0.03 | 0.32‡ | 0.15‡ | 0.56‡ | 0.43‡ | 0.30‡ | 0.38‡ | 0.63‡ | — | ||||
| 10. Goals | 0.04 | 0.31* | 0.16* | 0.49* | 0.43* | 0.36* | 0.37* | 0.54* | 0.50* | — | |||
| 11. Impulsivity | 0.04 | 0.26* | 0.17* | 0.49* | 0.37* | 0.27* | 0.29* | 0.60* | 0.51* | 0.62* | — | ||
| 12. Strategies | 0.10‡ | 0.33* | 0.16* | 0.69* | 0.50* | 0.32* | 0.37* | 0.74* | 0.66* | 0.65* | 0.71* | — | |
| 13. Clarity | 0.11‡ | 0.24* | 0.15* | 0.56* | 0.38* | 0.24* | 0.23* | 0.57* | 0.50* | 0.41* | 0.46* | 0.57* | — |
| Mean | 32.28 | 16.90 | 3.67 | 13.40 | 34.17 | 16.32 | 18.17 | 17.26 | 2.13 | 2.22 | 1.62 | 1.86 | 2.11 |
| SD | 7.92 | 10.76 | 4.02 | 10.54 | 14.73 | 7.01 | 8.92 | 8.99 | 0.99 | 0.84 | 0.69 | 0.76 | 0.78 |
| Range | 17–54 | 0–49 | 0–31 | 0–60 | 17–85 | 8–49 | 0–44 | 7–49 | 1–5 | 1–5 | 1–5 | 1–5 | 1–5 |
*p < 0.05.
†p < 0.01.
‡p < 0.001.
Alcohol use problems, Alcohol Use Disorders Identification Test (AUDIT); BMI, body mass index; Depressive symptoms, Beck Depression Inventory (BDI); Health complaints, Pennebaker Inventory of Limbic Languidness (PILL); Nonacceptance, Goals, Impulsivity, Strategies, Clarity, Difficulties in Emotion Regulation Scale (DERS); Peritraumatic dissociation, Peritraumatic Dissociative Experiences Questionnaire (PDEQ); Peritraumatic distress, Peritraumatic Distress Inventory (PDI); Psychological inflexibility, Acceptance and Action Questionnaire (AAQ); PTSD, Posttraumatic Stress Disorder, Posttraumatic Checklist (PCL); SD, standard deviation.
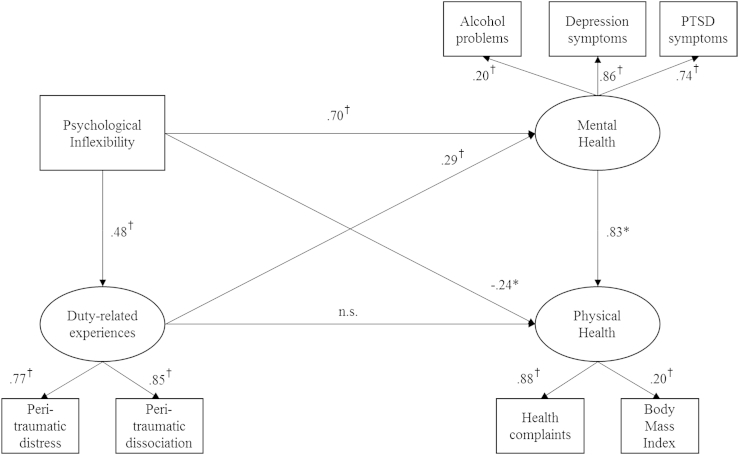
Notably, the physical health variables differed as a function of gender, age, and years of experience. Specifically, weight category (i.e., normal weight, overweight, obese) worsened with age [F(2,626) = 3.26, p = 0.04) and years of experience [F(2,626) = 3.35, p = 0.04). A Chi-square analysis [χ2(2) = 8.44, p = 0.02] revealed that men were over-represented in the obese category while women were over-represented in the overweight and normal weight categories. When compared to men, women reported more physical health complaints [t(756) = 5.52, p < 0.001). No association was found between physical health complaints and age (r = −0.02, p = 0.63) or years of experience (r = −0.01, p = 0.82). However, inclusion of age, gender, and years of experience as covariates in the models described below resulted in no changes to the significance of neither the model fit, nor the significance or direction of the observed pathways. As such, these covariates were not included in the final models. Two structural equation models were tested using IBM SPSS AMOS (version 22). The first model examined psychological inflexibility, duty-related distress and dissociation, mental health, and physical health (e.g., BMI and physical health complaints; Fig. 1). The model demonstrated adequate fit [χ2 (15) = 100.49, p < 0.001; normed fit index = 0.95, comparative fit index = 0.96; and root mean square error of approximation = 0.08). As anticipated, greater psychological inflexibility had a direct positive effect on duty-related experiences and mental health, and mental health had a direct effect on physical health. Contrary to predictions, however, duty-related experiences did not have a direct effect on physical health. Further, the direction of the significant direct effect of psychological inflexibility on physical health was in the negative direction. Said differently, as psychological inflexibility increased, physical health problems decreased.
Fig. 1.
Structural equation model examining psychological inflexibility and duty-related experiences as a predictor of physical health problems. PTSD, posttraumatic stress disorder. *p < 0.05, †p < 0.001.
A number of significant indirect effects were identified using 5,000 bootstrapped samples with replacement and 95% confidence intervals (CIs) around the estimated effect. To begin, though duty-related experiences failed to show a direct effect on physical health, an indirect effect of this latent variable on physical health was demonstrated via adverse mental health (95% CI: 0.14–0.40, p < 0.001). Further, psychological inflexibility had an indirect effect on adverse mental health via greater duty-related distress and dissociation (95% CI: 0.10–0.19, p < 0.001). Finally, psychological inflexibility had a total indirect effect on physical health via pathways through adverse mental health and duty-related experiences and mental health (95% CI: 0.49–1.05, p < 0.001).
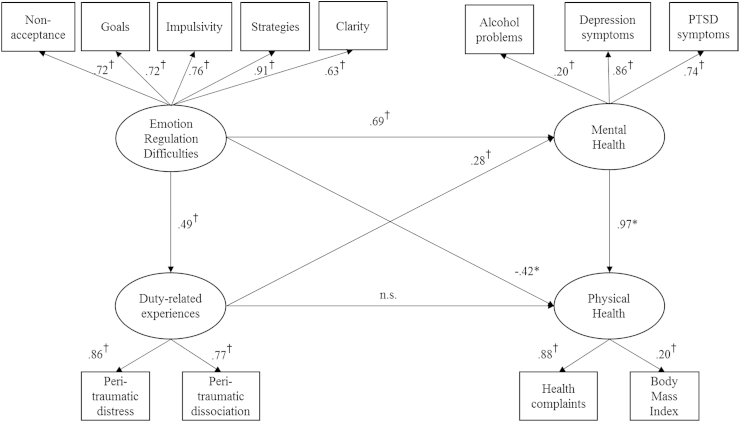
A second structural equation model was tested with emotion regulation difficulties, as estimated by five subscales of the DERS (Fig. 2), and demonstrated adequate fit [χ2 (48) = 262.33, p < 0.001; normed fit index = 0.94, comparative fit index = 0.94; root mean square error of approximation = 0.07]. A similar pattern of results was revealed for the model with the same unanticipated findings; namely, no direct effect of duty-related experiences on physical health was found, and a significant direct effect in the negative direction was observed between emotion regulation difficulties and physical health. As emotion regulation difficulties increased, physical health problems decreased. In regard to indirect effects, duty-related experiences had a significant indirect effect on physical health problems via adverse mental health (95% CI: 0.15–0.45, p < 0.001), and emotion regulation difficulties had an indirect effect on adverse mental health via duty-related experiences (95% CI: 0.09–0.19, p < 0.001). Finally, emotion regulation difficulties had a total indirect effect on physical health via a pathway through adverse mental health and a pathway through duty-related experiences and mental health (95% CI: 0.59–1.18, p < 0.001).
Fig. 2.
Structural equation model examining emotion regulation difficulties and duty-related experiences as a predictor of physical health problems. PTSD, posttraumatic stress disorder. *p < 0.05, †p < 0.001.
4. Discussion
One of the primary aims of this study was to examine the extent of obesity and physical health complaints among 911 telecommunicators, a population that has received scant empirical attention despite being at high-risk for adverse health given the work environment and demands of this occupation. Rates of obesity in the sample (53.4%) were 50% greater than the national prevalence rate (34.9%) [52], and less than one in five telecommunicators fell into the normal weight category. These rates are roughly equivalent to those identified in firefighters (78.4–79.5%) [19]. On average, telecommunicators reported experiencing nearly 17 different physical health complaints at least once a month, and up to daily. The most commonly reported physical health complaint was headaches, followed by back pains, insomnia/difficulty sleeping, stiff or sore muscles, itchy eyes or skin, and heartburn. These physical health ailments make sense in relation to the 911 work environment, as chronic exposure to computer screens can lead to headaches and itchy/watery eyes, remaining seated for long periods can results in stiff/sore muscles and exacerbate back pain, and shift work schedules can result in insomnia/difficulty sleeping. Stress and distress may also result in recurrent headaches, skeletal–muscular pain, heartburn, and insomnia. Notably, the zero order correlations revealed that greater physical health complaints were strongly related to depressive symptoms, alcohol abuse, PTSD symptoms, psychological inflexibility, and emotion dysregulation, as well as greater peritraumatic distress and dissociation.
A secondary aim of the present study was to identify predictors of poor physical health (e.g., BMI and physical health complaints) in this population. Structural equation modeling identified several important direct and indirect predictors of the physical health outcome variables. Psychological health, which was estimated by alcohol use problems, depressive symptoms, and PTSD symptoms, had a strong and direct effect on physical health. This replicates on a longstanding empirical literature that connects psychological and physical health functioning [53], [54], [55]. Notably, peritraumatic reactions to one's worst duty-related event did not have a direct effect on physical health, but instead, had an indirect influence through the development of adverse psychological health. These results suggest that early intervention and continued assessment of psychological functioning in the aftermath of a particularly distressing call may have protective effects on physical health through reductions in psychological pathology.
Indirect effects on physical health were also observed for emotion dysregulation and psychological inflexibility. Namely, emotion dysregulation had an indirect effect on the physical health outcome variables by enhancing the risk for greater peritraumatic distress and dissociation reactions, which heightened rates of poor mental health. Emotion dysregulation also had a direct effect on mental health and an indirect effect on physical health through poor mental health.
The same relationships were observed for psychological inflexibility. The results indicate that the impact of emotion dysregulation and psychological inflexibility on physical health is at least partially accounted for by the effect of these constructs on psychopathology. However, a curious finding was observed in that emotion dysregulation and psychological inflexibility had a negative direct effect on physical health in the full structural equation modeling models, suggesting that greater dysregulation and inflexibility was associated with fewer physical health problems. It is possible that controlling for the impact of duty-related peritraumatic reactions and poor mental health on physical health allows one to observe a unique and interesting relationship between emotional responding and physical health. Research from the coping literature has repeatedly argued for the importance of considering context when determining whether a particular strategy is, or should be, effective in reducing distress [56]. Telecommunicators are tasked with handling calls effectively and efficiently, regardless of the call content. This often requires a telecommunicator to remain calm and stifle their own emotional reactions to a potentially distressing call. Further, telecommunicators are trained to handle calls according to protocols that are standardized. Failure to use the protocols appropriately can result in reprimand for the employee, and potentially a tragedy if the call is not handled properly. As such, the work environment and job demands can engender greater reliance of a small subset of emotion regulation strategies such as suppression or avoidance, and greater inflexibility over time. Though this does seem to enhance the risk for poor functioning in both the psychological and physical domains, the results suggest that these factors are not problematic in the absence of psychopathology. Said differently, emotion dysregulation and psychological inflexibility are only problematic in regard to physical health to the extent that they enhance risk for psychopathology. However, if one can remain psychologically healthy, perhaps through use of protective factors not considered in this study (i.e., social support, spirituality, psychological intervention) [57], [59], [58], reliance of these forms of coping may actually be adaptive in this work environment and reduce risk for poor physical health. Another possibility is that the negative relationship is simply a spurious finding—an artifact of using structural equation modeling.
The results of this study have several implications for prevention and intervention efforts. Notably, many of the observed effects on the physical health outcome variables occurred through mental health functioning. This suggests that targeting mental health functioning may have a direct, salutatory effect on physical health. To begin, early intervention after particularly stressful or “hot” calls is recommended. Early intervention in the form of Critical Incident Stress Management (CISM) has been used in 911 call centers per anecdotal report, however, 911 telecommunicators are not always invited to debriefings among the other responders involved in a particularly distressing emergency. Furthermore, there is some evidence to suggest that CISM can have negative long-term effects for those who participate in debriefings, particularly if the debriefing is mismanaged or employees are required to attend [60]. As such, CISM should not be mandatory for employees and call centers should rely on well-trained interventionists to carry out the program. In addition to CISM, it is important to recognize that physical health problems among 911 employees may be indicative of greater psychological suffering. It is possible that physical suffering is the language used by telecommunicators when they are suffering more generally. This would be consistent with other emergency responders, such as police officers, who may be more willing to recognize or admit when they have a physical health ailment in comparison to a psychological health problem [29]. As such, recurrent reports of physical health ailments made by 911 telecommunicators may be worthy of a more extensive assessment and consideration.
Prevention and intervention efforts must be adapted for this population, as their work environment and job demands are unique relative to other emergence responders and the general population. As suggested by this study's results, what is considered pathological in regard to emotion dysregulation and psychological inflexibility may actually be adaptive among some telecommunicators, particularly if these characteristics are present among psychologically healthy telecommunicators. Encouraging psychologically healthy telecommunicators to be more flexible or emotionally attuned could impair their job performance, or affect their health if they begin “taking work home with them.”
At the same time, emotion dysregulation and psychological inflexibility did have a significant effect on mental health, and furthermore, these constructs had an impact on physical health via mental health. Some telecommunicators may therefore benefit from prevention and intervention efforts that target emotion dysregulation and psychological inflexibility. Components of Mindfulness-based Stress Reduction [61] and Acceptance and Commitment Therapy [62] may be two viable options for adapted prevention and intervention with this population that target emotion dysregulation and psychological inflexibility. Empirical support and use of these approaches is a more recent phenomenon, however, both have been used to alleviate a myriad of psychological (i.e., PTSD, depression, anxiety) and physical (i.e., pain) ailments at the intervention stage [61], [63], [65], [64]. Furthermore, there is conceptual support for the use of mindfulness and acceptance-based approaches in resiliency training for individuals at high-risk for trauma exposure [66]. In addition, prevention efforts that provide psychoeducation on the potential impact of duty-related stress and distress may help telecommunicators identify when they are in need of intervention from a physician or mental health professional.
It was found that age and years of experience took a toll on participants' weight. As participants aged and remained in the career, their BMI significantly increased. The results point to the importance of continued prevention and intervention efforts as telecommunicators age and/or remain in the career. As an occupation with a largely sedentary work description, it is important to offer opportunities for telecommunicators to make healthy choices in regard to physical movement, eating, and sleep patterns. The use of work incentives to participate in exercise programs and/or healthy eating programs may be a first step in fighting the obesity epidemic in this population. Proactive measures such as psychoeducation for trainees and those early in their career may also help prevent unhealthy weight gain.
The present study is the first known study to examine physical health and its predictors among 911 telecommunicators. The conclusions must be considered in light of the study limitations. The study used a cross-sectional design, which limits the conclusions that can be drawn regarding temporal sequencing. It is possible, for instance, that physical health problems lead to mental health problems, or that the presence of poor health affects duty-related experiences when presented with a “hot” call. As such, the conclusions from this study should be replicated with a longitudinal design. Furthermore, though the sample size was large, the use of convenience sampling and the recruitment strategies could have resulted in a nonrepresentative sample of telecommunicators. We were unable to identify data on the distribution of demographic factors among 911 telecommunicators, and therefore, whether our sample is representative of the population cannot be determined. Participants who initially indicated interest, but who did not participate in the survey, did not provide the researchers with any demographic information. As such, we are also unable to determine whether these individuals differed significantly from our sample. In addition, the sample consisted of telecommunicators who had remained in the 911 field for at least 1 year, with the mean years of experience recorded at >12 years. This may be indicative of a relatively hardy and resilient sample of telecommunicators, as they have continued to remain in a high stress occupation and have not attrited from the occupation due to poor performance or functioning. Future research using a prospective design that includes a representative sample of telecommunicators could further inform the field and provide more rigorous conclusions regarding causal relationships, as well as more accurate point estimates of poor health in this population.
An additional limitation to the study is the use of self-reporting to determine rates of obesity. BMI was calculated based upon participants' self-reported height and weight. Although self-reported height may have a more limited margin of error, an individual's ability to estimate accurately one's weight may be less clear. However, a recent study found a strong correlation between an individual's weight as reported online and the individual's weight when measured in the lab [67]. In cases of discrepancy, it was more often the case that participants underestimated their weight online. As such, there may be reason to believe that the prevalence of overweight and obese individuals in the sample may have been even greater. To improve upon this study's methodology, future research would benefit from having participants complete a standardized physical examination to determine the true extent of obesity and physical illness among the population. This study examined only BMI and physical health complaints, which represents a narrow range of possible physical health outcomes. Despite the limitations of the study, results suggest a health crisis among this important sector of the emergency responding workforce, who play a critical role in the health and welfare of the general public. Development of adapted prevention and intervention efforts is an important next step in protecting the health of this valuable, at-risk population.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.Benedek D.M., Fullerton C., Ursano R.J. First responders: mental health consequences of natural and human-made disasters for public health and public safety workers. Annu Rev Public Health. 2007;28:55–68. doi: 10.1146/annurev.publhealth.28.021406.144037. [DOI] [PubMed] [Google Scholar]
- 2.Tsismenakis A.J., Christophi C.A., Burress J.W., Kinney A.M., Kim M., Kales S.N. The obesity epidemic and future emergency responders. Obesity. 2009;17:1648–1650. doi: 10.1038/oby.2009.63. [DOI] [PubMed] [Google Scholar]
- 3.Bacharach S.B., Bamberger P.A., Doveh E. Firefighters, critical incidents, and drinking to cope: the adequacy of unit-level performance resources as a source of vulnerability protection. J Appl Psychol. 2008;93:155–169. doi: 10.1037/0021-9010.93.1.155. [DOI] [PubMed] [Google Scholar]
- 4.Carey M.G., Al-Zaiti S.S., Dean G.E., Sessanna L., Finnell D.S. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J Occup Environ Med. 2012;53:928–933. doi: 10.1097/JOM.0b013e318225898f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ballenger J.F., Best S.R., Metzler T.J., Wasserman D.A., Mohr D.C., Liberman A., Marmar C.R. Patterns and predictors of alcohol use in male and female urban police officers. Am J Addict. 2011;1:21–29. doi: 10.1111/j.1521-0391.2010.00092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Violanti J.M., Slaven J.E., Charles L.E., Burchfiel C.M., Andrew M.E., Homish G.G. Police and alcohol use: A descriptive analysis and associations with stress outcomes. Am J Crim Justice. 2011;36:344–356. [Google Scholar]
- 7.Osofsky H.J., Osofsky J.D., Arey J., Kronenberg M.E., Hansel T., Many M. Hurricane Katrina’s first responders: the struggle to protect and serve in the aftermath of the disaster. Disaster Med Public Health Prep. 2011;5:214–219. doi: 10.1001/dmp.2011.53. [DOI] [PubMed] [Google Scholar]
- 8.Meyer E.C., Zimering R., Daly E., Knight J., Kamholz B.W., Gulliver S.B. Predictors of posttraumatic stress disorder and other psychological symptoms in trauma-exposed firefighters. Psychol Serv. 2012;9:1–15. doi: 10.1037/a0026414. [DOI] [PubMed] [Google Scholar]
- 9.Wang Z., Inslicht S.S., Metzler T.J., Henn-Haase C., McCaslin S., Tong H., Marmar C.R. A prospective study of depression symptoms in police. Psychiatry Res. 2010;175:211–216. doi: 10.1016/j.psychres.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biggs Q.M., Fullerton C.S., Reeves J.J., Grieger T.A., Reissman D., Ursano R.J. Acute stress disorder, depression, and tobacco use in disaster workers following 9/11. Am J Orthopsychiatry. 2010;80:586–592. doi: 10.1111/j.1939-0025.2010.01063.x. [DOI] [PubMed] [Google Scholar]
- 11.Galatzer-Levy I., Madan A., Neylan T., Henn-Haase C., Marmar C. Peritraumatic and trait dissociation differentiate police officers with resilient versus symptomatic trajectories of posttraumatic stress symptoms. J Trauma Stress. 2011;24:557–565. doi: 10.1002/jts.20684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perrin M.A., DiGrande L., Wheeler K., Thorpe L., Farfel M., Brackbill R. Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers. Am J Psychiatry. 2007;164:1385–1394. doi: 10.1176/appi.ajp.2007.06101645. [DOI] [PubMed] [Google Scholar]
- 13.Pierce H., Lilly M.M. Duty-related trauma exposure in 911 telecommunicators: considering the risk for posttraumatic stress. J Trauma Stress. 2012;25:211–215. doi: 10.1002/jts.21687. [DOI] [PubMed] [Google Scholar]
- 14.Taylor M. APCO Project RETAINS: responsive efforts to address integral needs in staffing. Paper presented at the Regional Conference of the Association of Public Safety Communications Officials. Kansas City (MO); 2005.
- 15.Troxell R. 2008. Indirect exposure to the trauma of others: the experiences of 911 telecommunicators. (Doctoral dissertation). Retried from ProQuest Dissertations and Theses database. Publication no.: 3335425. [Google Scholar]
- 16.Sparks K., Cooper C., Fried Y., Shirom A. The effects of hours of work on health: a meta-analytic review. J Occup Organ Psychol. 2011;70:391–408. [Google Scholar]
- 17.Violanti J.M., Burchfiel C.M., Hartley T.A., Mnatsakanova A., Fekedulegn D., Andrew M.E., Vila B.J. Atypical work hours and metabolic syndrome among police officers. Arch Environ Occup Health. 2009;64:194–201. doi: 10.1080/19338240903241259. [DOI] [PubMed] [Google Scholar]
- 18.Donovan R., Nelson T., Peel J., Lipsey T., Voyles W., Israel R.G. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med. 2009;59:487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- 19.Poston W.S.C., Haddock K., Jahnke S.A., Jitnarin N., Tuley B.C., Kales S.N. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med. 2011;53:266–273. doi: 10.1097/JOM.0b013e31820af362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yeomans M.R. Alcohol, appetite and energy balance: is alcohol intake a risk factor for obesity? Physiol Behav. 2010;100:82–89. doi: 10.1016/j.physbeh.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 21.Stunkard A., Faith M., Allison M. Depression and obesity. Biol Psychiatry. 2003;54:330–332. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 22.Gu J.K., Charles L.E., Burchfiel C.M., Andrew M.E., Ma C., Bang K.M., Violanti J.M. Associations between psychological distress and body mass index among law enforcement officers; the National Health Interview Survey 2004–2010. Saf Health Work. 2013;4:52–62. doi: 10.5491/SHAW.2013.4.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman M.J., Schnurr P. The relationship between trauma, post-traumatic stress disorder, and physical health. In: Friedman M.J., Charney D.S., Deutch A.Y., editors. Neurobiological and clinical consequences of stress: from normal adaptation to post-traumatic stress disorder. Lippincott-Raven; Philadelphia (PA): 1995. pp. 507–524. [Google Scholar]
- 24.Violanti J.M., Fekedulegn D., Hartley T.A., Andrew M.E., Charles L.E., Mnatsakanova A., Burchfiel C.M. Police trauma and cardiovascular disease: association between PTSD symptoms and metabolic syndrome. Int J Emerg Ment Health. 2006;8:227–238. [PubMed] [Google Scholar]
- 25.Ozer E.J., Best S.R., Lipsey T.L., Weiss D.S. Predictors of posttraumatic stress disorder and symptoms in adults: a meat-analysis. Psychol Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- 26.Lilly M.M., Pierce H. PTSD and depressive symptoms in 911 telecommunicators: the role of peritraumatic distress and world assumptions in predicting risk. Psychol Trauma. 2012;5:135–141. [Google Scholar]
- 27.Marmar C.R., McCaslin S.E., Metzler T.J., Best S., Weiss D.S., Fagan J., Neylan T. Predictors of posttraumatic stress in police and other first responders. Ann N Y Acad Sci. 2006;1071:1–18. doi: 10.1196/annals.1364.001. [DOI] [PubMed] [Google Scholar]
- 28.Weiss D.S., Marmar C.R., Metzler T.J., Ronfeldt H.M. Predicting symptomatic distress in emergency services personnel. J Consult Clin Psychol. 1995;63:361–368. doi: 10.1037//0022-006x.63.3.361. [DOI] [PubMed] [Google Scholar]
- 29.Lilly M.M., Pole N., Best S.R., Metzler T., Marmar C.R. Gender and PTSD: what can we learn from female police officers? J Anxiety Disord. 2009;23:767–774. doi: 10.1016/j.janxdis.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gratz K.L., Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–44. [Google Scholar]
- 31.Boden M., Westermann S., McRae K., Kuo J., Alvarez J., Kulkarni M.R., Gross J.J., Bonn-Miller M.O. Emotion regulation and posttraumatic stress disorder: a prospective investigation. J Soc Clin Psychol. 2013;32:296–314. [Google Scholar]
- 32.Bonn-Miller M., Vujanovic A., Boden M., Gross J. Posttraumatic stress, difficulties in emotion regulation, and coping-oriented marijuana use. Cogn Behav Ther. 2011;40:34–44. doi: 10.1080/16506073.2010.525253. [DOI] [PubMed] [Google Scholar]
- 33.Tull M., Barrett H., McMillan E. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behav Ther. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 34.Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Gianini L., White M., Masheb R. Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eat Behav. 2013;14:309–313. doi: 10.1016/j.eatbeh.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kashdan T.B., Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. 2010;30:865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bonanno G.A., Papa A., Lalande K., Westphal M., Coifman K. The importance of being flexible. Psychol Sci. 2004;15:482–487. doi: 10.1111/j.0956-7976.2004.00705.x. [DOI] [PubMed] [Google Scholar]
- 38.Westphal M., Seivert N.H., Bonanno G.A. Expressive flexibility. Emotion. 2010;10:92–100. doi: 10.1037/a0018420. [DOI] [PubMed] [Google Scholar]
- 39.Berking M., Meier C., Wupperman P. Enhancing emotion-regulation skills in police officers: results of a pilot controlled study. Behav Ther. 2010;41:329–339. doi: 10.1016/j.beth.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 40.Pennebacker J.W. Putting stress into words: health, linguistic, and therapeutic implications. Behav Res Ther. 1993;31:539–548. doi: 10.1016/0005-7967(93)90105-4. [DOI] [PubMed] [Google Scholar]
- 41.Babor T.F., Higgins-Biddle J.C., Saunders J.B., Monteiro M.G. World Health Organization; Geneva (Switzerland): 2001. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for use in primary care. [Google Scholar]
- 42.Menard K.S., Arter M.L. Police officer alcohol use and trauma symptoms: associations with critical incidents, coping, and social stressors. Int J Stress Manag. 2013;20:37–56. [Google Scholar]
- 43.Beck A.T., Steer R.A., Brown G.K. Psychological Corporation; San Antonio (TX): 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- 44.Marchand A., Durand P. Psychological distress, depression, and burnout: Similar contribution of the job demand-control and job demand-control-support models. J Occup Env Med. 2011;53:185–189. doi: 10.1097/JOM.0b013e318206f0e9. [DOI] [PubMed] [Google Scholar]
- 45.Brouwer D., Meijer R.R., Zevalkink J. On the factor structure of the Beck Depression Inventory-II: G is the key. Psychol Assess. 2013;25:136–145. doi: 10.1037/a0029228. [DOI] [PubMed] [Google Scholar]
- 46.Ruggiero K.J., Del Ben K., Scotti J.R., Rabalais A.E. Psychometric properties of the PTSD Checklist—Civilian Version. J Trauma Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- 47.Brunet A., Weiss D.S., Metzler T.J., Best S.R., Neylan T.C., Rogers C., Marmar C.R. The Peritraumatic Distress Inventory: a proposed measure of PTSD criterion A2. Am J Psychiatry. 2001;158:1480–1485. doi: 10.1176/appi.ajp.158.9.1480. [DOI] [PubMed] [Google Scholar]
- 48.Marmar C.R., Metzler T.J., Otte C. 2nd ed. Guilford Press; New York (NY): 2004. The Peritraumatic Dissociative Experiences Questionnaire Assessing psychological trauma and PTSD; pp. 144–167. [Google Scholar]
- 49.Maia D.B., Marmar C.R., Henn-Haase C., Nobrega A., Fiszman A., Marques-Portella C., Figueira I. Predictors of PTSD symptoms in Brazilian police officers: the synergy of negative affect and peritraumatic dissociation. Rev Bras Psiquiatr. 2011;33:362–366. doi: 10.1590/s1516-44462011000400009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gratz K.L., Dixon-Gordon K.L., Tull M.T. Predictors of treatment response to an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Personal Disord. 2014;5:97–107. doi: 10.1037/per0000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bond F.W., Hayes S.C., Baer R.A., Carpenter K.M., Guenole N., Orcutt H.K., Zettle R.D. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011;42:676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 52.Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. J Am Med Assoc. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dickey B., Normand S.T., Weiss R.D., Drake R.E., Azeni H. Medical morbidity, mental illness, and substance use disorders. Psychiatr Serv. 2002;53:861–867. doi: 10.1176/appi.ps.53.7.861. [DOI] [PubMed] [Google Scholar]
- 54.Howell R.T., Kern M.L., Lyubomirsky S. Health benefits: meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol Rev. 2007;1:83–136. [Google Scholar]
- 55.Jones D.R., Macias C., Barreira P.J., Fisher W.H., Hargreaves W.A., Harding C.M. Prevalence, severity, and co-occurrence of chronic health problems of persons with serious mental illness. Psychiatr Serv. 2004;55:1250–1257. doi: 10.1176/appi.ps.55.11.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lazarus R.S., Folkman S. Transactional theory and research on emotions and coping. Eur J Personality. 1987;1:141–169. [Google Scholar]
- 57.Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 58.Unterrainer H.F., Lewis A.J., Fink A. Religious/spiritual well-being, personality and mental health: a review of results and conceptual issues. J Relig Health. 2014;53:382–392. doi: 10.1007/s10943-012-9642-5. [DOI] [PubMed] [Google Scholar]
- 59.Wheeler R.J., Frank M.A. Identification of stress buffers. Behav Med. 1988;14:78–89. doi: 10.1080/08964289.1988.9935128. [DOI] [PubMed] [Google Scholar]
- 60.Everly G.S., Flannery R.B., Mitchell J.T. Critical incident stress management (CISM): a review of the literature. Aggress Violent Beh. 2000;5:23–40. [Google Scholar]
- 61.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clin Psychol Sci Pract. 2003;10:144–156. [Google Scholar]
- 62.Hayes S.C., Strosahl K., Wilson K.G. Guilford Press; New York (NY): 1999. Acceptance and commitment therapy: An experiential approach to behavior change. [Google Scholar]
- 63.Orsillo S.M., Roemer L. Guilford Press; New York (NY): 2011. The mindful way through anxiety: break free from chronic worry and reclaim your life. [Google Scholar]
- 64.Segal Z.V., Williams J.M.G., Teasdale J.D. Guilford Press; New York (NY): 2002. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. [Google Scholar]
- 65.Walser R.D., Westrup D. New Harbinger Publications; Oakland (CA): 2007. Acceptance & commitment therapy for the treatment of Post-traumatic Stress Disorder. [Google Scholar]
- 66.Thompson R.W., Arnkoff D.B., Glass C.R. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma Violence Abuse. 2011;12:220–235. doi: 10.1177/1524838011416375. [DOI] [PubMed] [Google Scholar]
- 67.Bonn S.E., Lagerros Y.T., Bälter K. How valid are web-based self-reports of weight? J Med Internet Res. 2013;15:e52. doi: 10.2196/jmir.2393. [DOI] [PMC free article] [PubMed] [Google Scholar]